THE UPLIFT INNOVATION PROGRAM

Amgen and IFPA invite psoriatic disease-focused patient organizations from around the world to participate in the UPLIFT Innovation Program. Leveraging findings from the UPLIFT survey, the initiative aims to make a big impact by developing solutions to a challenge that people with psoriatic disease and their healthcare providers continue to face.
THE PROGRAM QUESTION
How can we boost collaboration between people living with psoriatic disease and their healthcare providers to establish and achieve shared treatment goals?
Who can participate?

All psoriatic disease-focused patient organizations from around the world. Application opens July 1.
Submission Deadline

Application closes Monday, August 14 at 23:59 Eastern Daylight Time.
2023 Grant

UPLIFT dedicates up to $100,000 USD for qualifying projects. Successful applicants will be announced in Fall 2023.
For more information about the judging panel and selection criteria, please download our application guidelines.
Do you have more questions? Click to view the FAQs.
Click to view the Terms & Conditions.
the disconnect
Key Takeaways from the UPLIFT Survey
Findings from the UPLIFT survey identified persistent unmet needs for people living with plaque psoriasis and/or psoriatic arthritis. This means that patients felt that they were not on the same page as their doctor around topics like:
Disease severity
Disease burden of special areas
Treatment goals
Disease Severity
Doctors determine how severe someone’s psoriasis is by using standard severity assessment measures, like Body Surface Area (BSA),1,‡ which calculates how much of your skin is affected by psoriasis. The more skin that’s affected, the higher the BSA and the more severe the psoriasis is considered. However, people living with psoriasis who had limited skin involvement – meaning only a small amount of their skin is affected by psoriasis – viewed their disease as more severe than was categorized by their doctors:
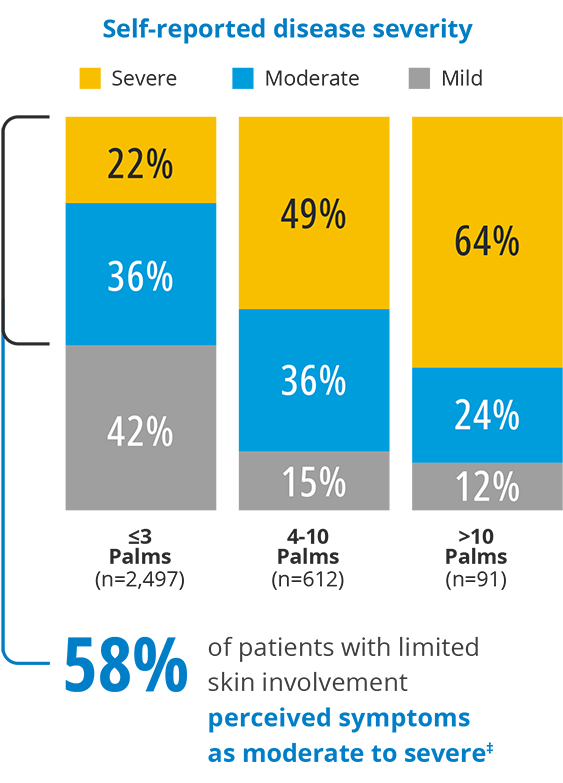
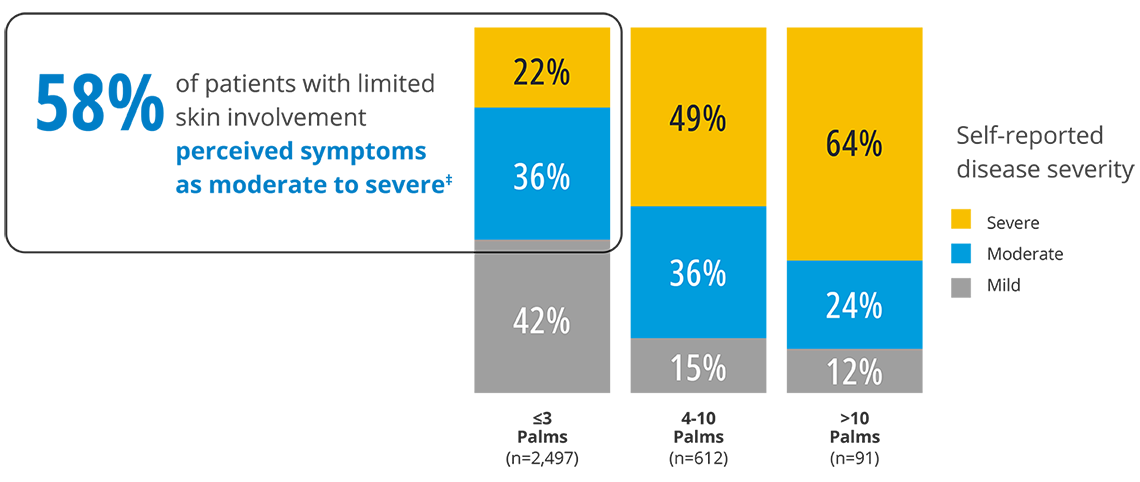
Patients and doctors evaluate disease severity differently
In fact, the amount of skin affected by psoriasis wasn’t even a top factor for people when considering their own disease severity.
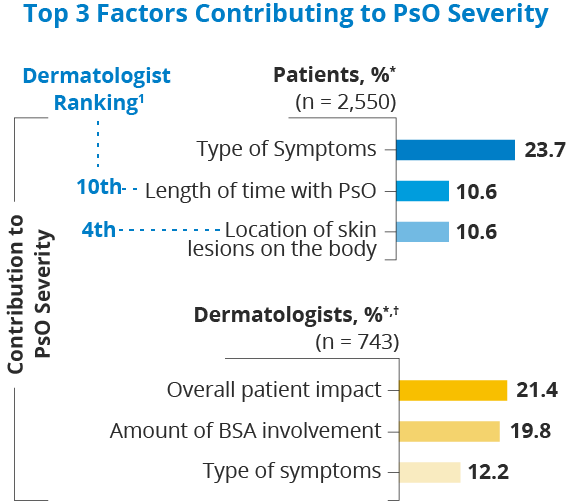
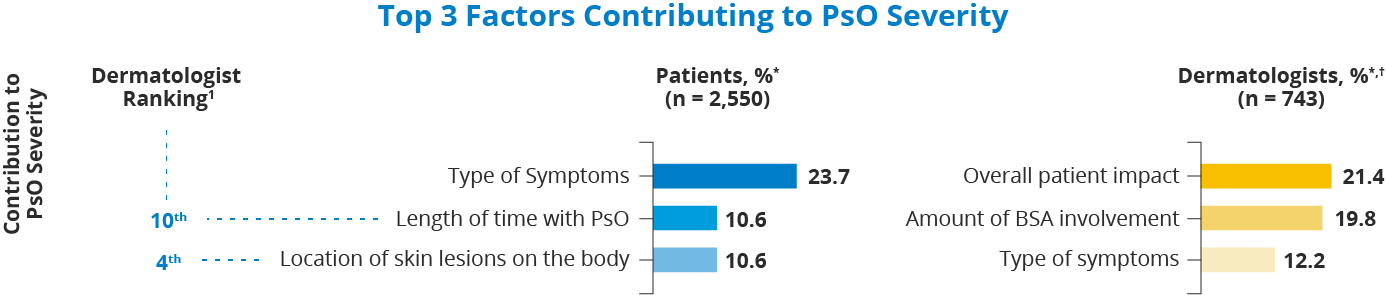
*Highest-ranking responses were calculated using the sum of scores. Percentages were calculated by dividing the sum of scores by the maximum possible score; † For “top 3 treatment goals,” separate responses were provided regarding patients in different BSA categories (mild, moderate, or severe). Shown is the aggregate of the 3 categories.
1. Reich K, et al. Presented at: 30th European Academy of Dermatology and Venereology (EADV) Congress; September 29–October 2, 2021; virtual. Oral Presentation FC03.01;
2. Lebwohl MG, et al. Dermatol Ther (Heidelb). 2021:1-16.
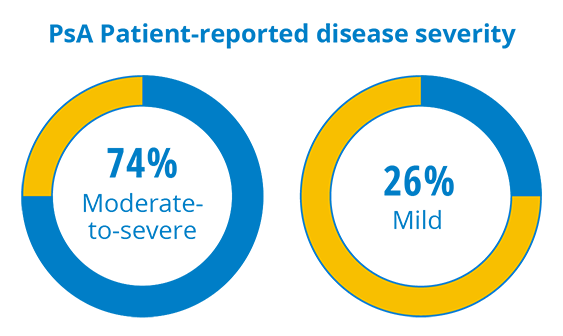
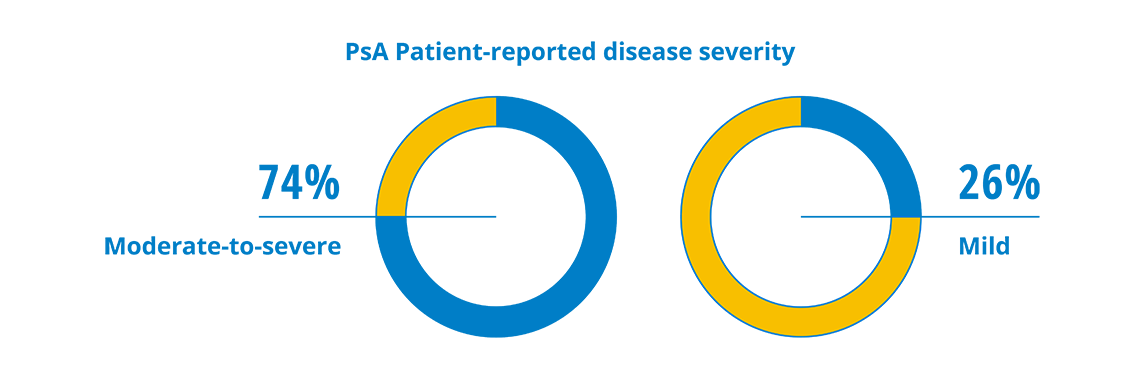
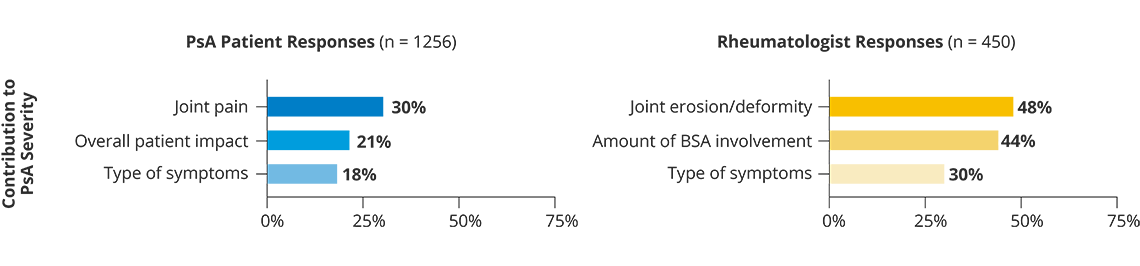
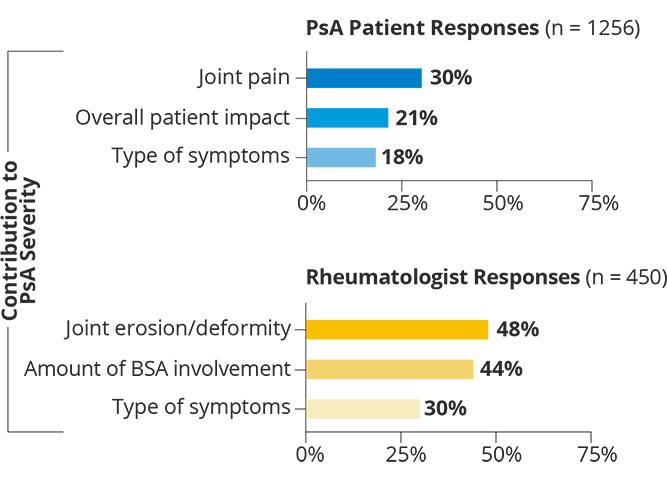
Like psoriasis, psoriatic arthritis can range from mild to severe and the severity is determined by how many joints in the body are affected. Although nearly half of people with PsA surveyed only had limited joint involvement (meaning fewer than four joints affected), disease burden and patient-perceived severity were high. Almost ¾ of people with PsA considered their PsA to be moderate-to-severe, despite most receiving treatment; yet only half had seen a doctor in the past year.
Disease Burden Of Special Areas
For patients in this survey, where psoriasis affected them was more of a concern than how much of their skin is affected. Psoriasis frequently appears in special areas such as the scalp, face, palms and/or soles, nails, and genitals, regardless of BSA:
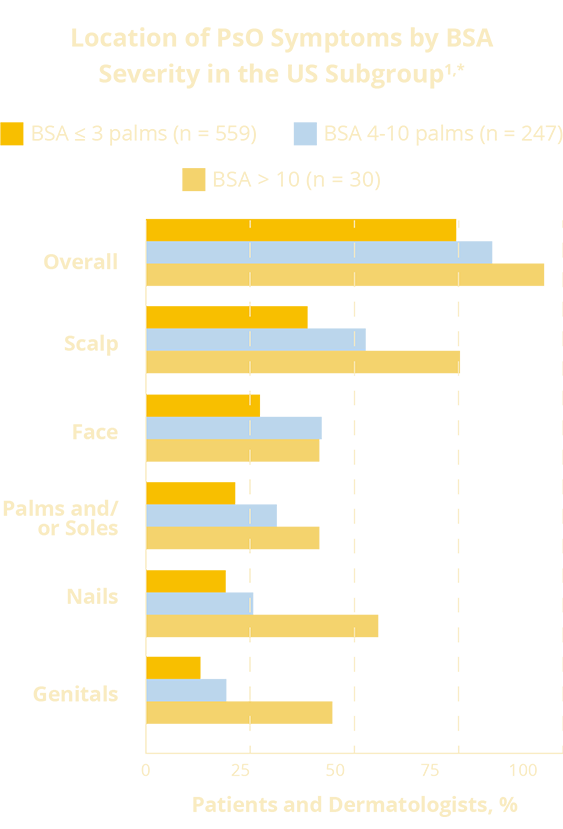
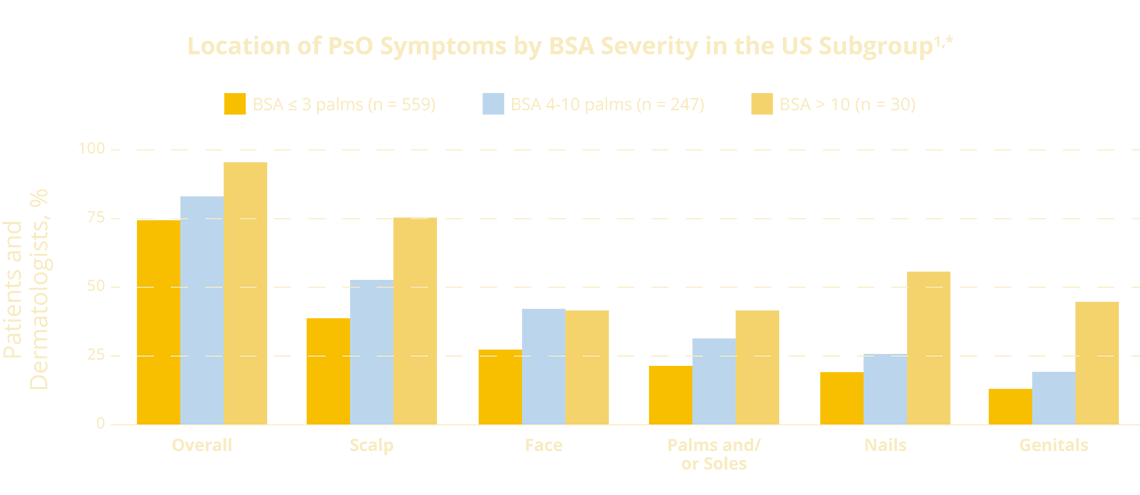
*Patients with PsO (PsO ± PsA) who are currently experiencing PsO symptoms. A Patient may have more than one special area.
1. Lebwohl MG, et al. Poster presented at: Maui Derm for Dermatologists; January 25-January 29, 2021; Maui, Hawaii; 2. Strober B, et al. J Am Acad Dermatol. 2020;82:117-122.
Among patients with low BSA and who are affected in at least one special area, three out of five consider their disease to be moderate or severe.
Treatment Goals
Nearly a third of people with psoriasis remain untreated, regardless of the extent of skin involvement. Almost 30% of people across severities (mild, moderate or severe) are on topicals only, but three quarters of patients with PsO and/or PsA consider topical treatments which was associated with a higher impact of disease burden.
Joint pain in people with PsO could be a sign of undiagnosed PsA. Compared with people with diagnosed PsA, people with PsO without a PsA diagnosis who reported joint pain were not treated with systemic therapy.
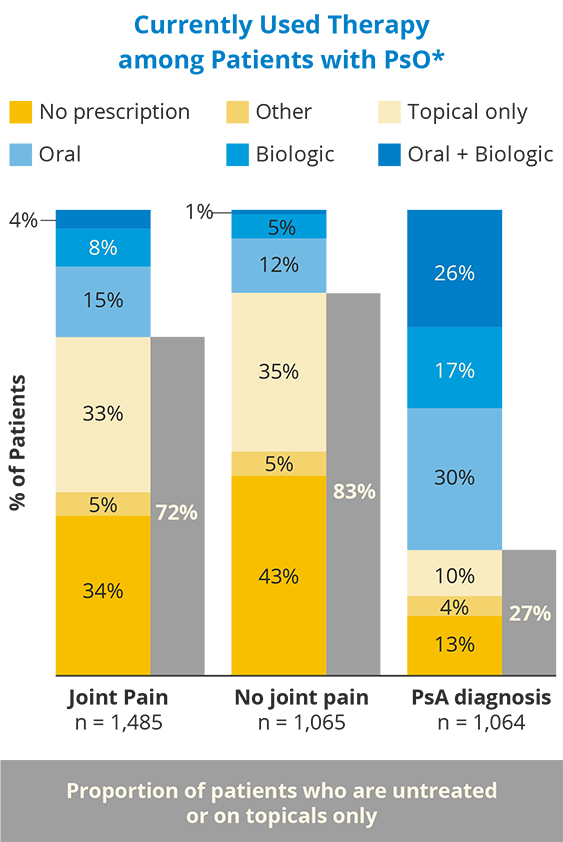
72% of patients with joint pain were not currently prescribed systemic therapy, compared with 27% of patients with a PsA diagnosis.
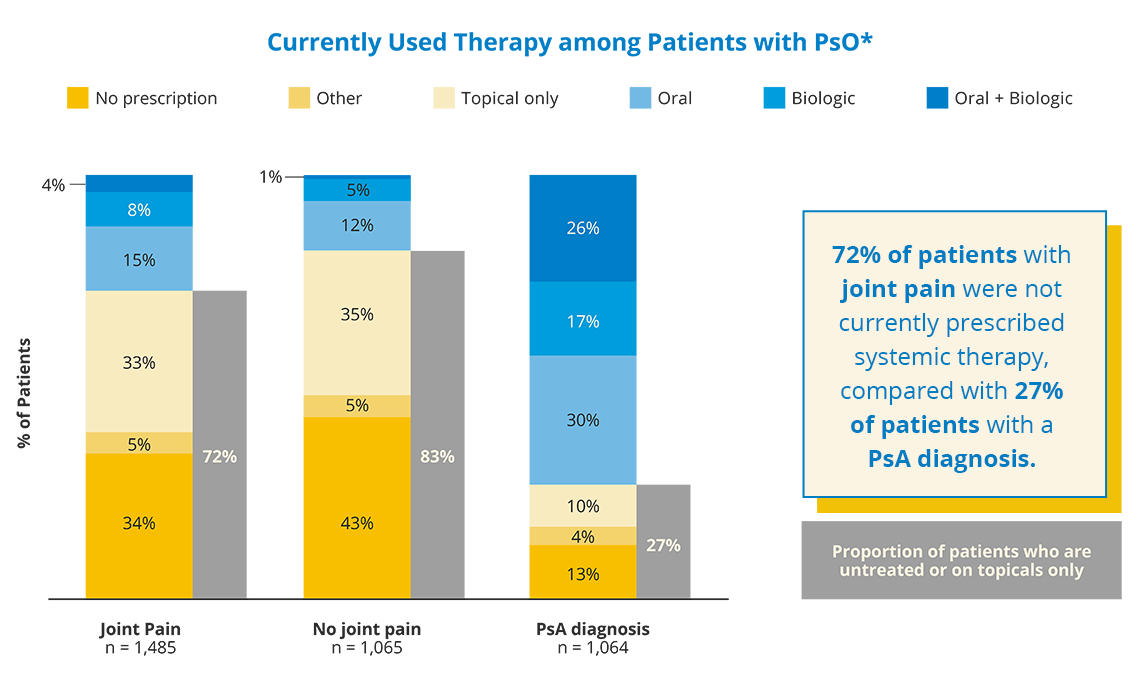
*Oral + Biologic: oral Rx + biologic ± topical Rx; Biologic: biologic ± topical Rx; Oral: oral Rx ± sensitivity–analysis topical Rx; Topical: topical Rx only; Other: other only, phototherapy only, or phototherapy + other (ie, anything other than prescription oral/biologic/topical therapy or phototherapy); No treatment: no treatment other than oral OTC or topical OTC.
Merola JF, et al. Poster presented at: 30th European Academy of Dermatology and Venereology (EADV) Congress; September 29–October 2, 2021; virtual. Poster P1465.
Patients and doctors sometimes have very different recollections of their office visits, which can make the disconnect feel even greater. Patients recalled fewer discussions of a range of topics, including joint involvement, and other related conditions.
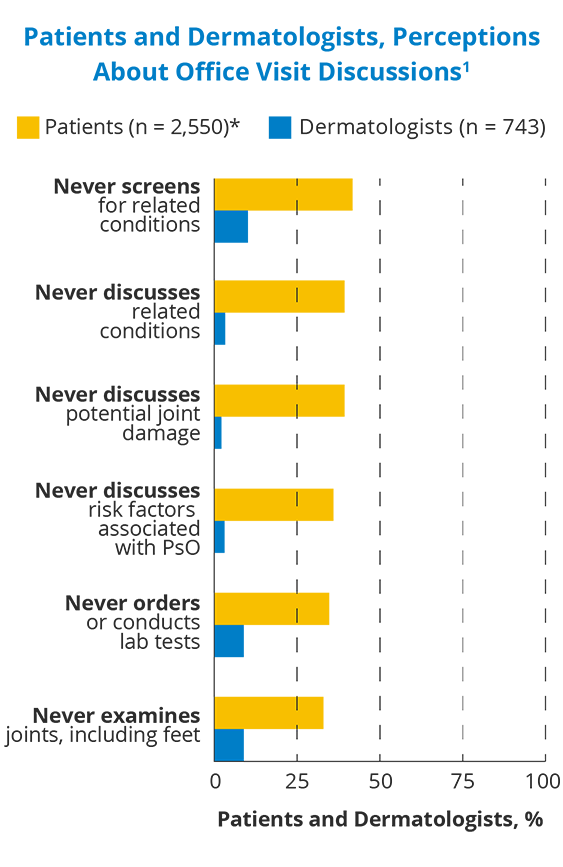
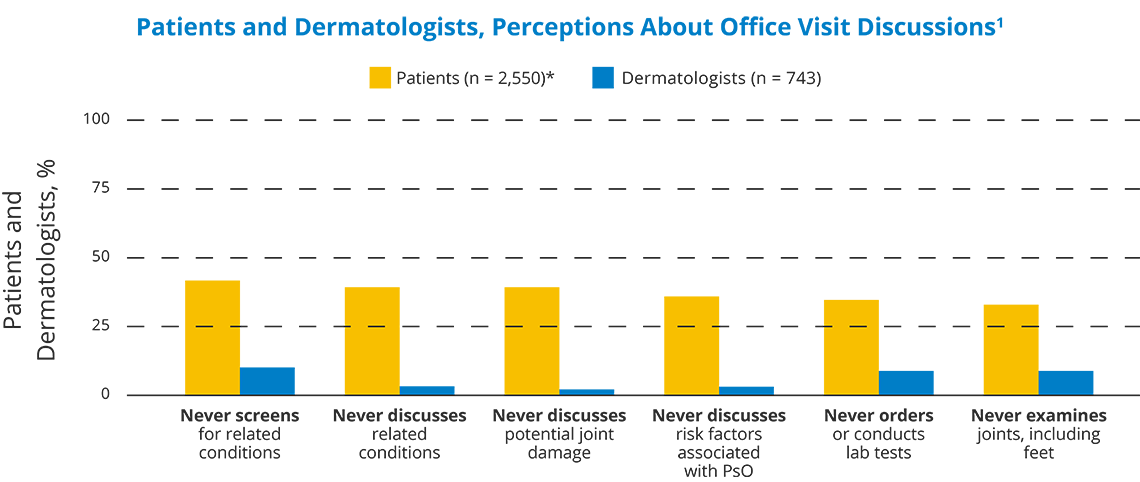
*Of 2,550 patients with PsO, 786 reported they visited the dermatologist and answered this question.
1. Lebwohl MG, et al. Dermatol Ther (Heidelb). 2021:1-16; 2. Reich K, et al. Presented at: 30th European Academy of Dermatology and Venereology Congress; September 29–October 2, 2021; virtual. Oral presentation FC03.01.
And while there’s some overlap in treatment goals between patients and doctors, there’s still a disconnect in the priority of these goals: 1
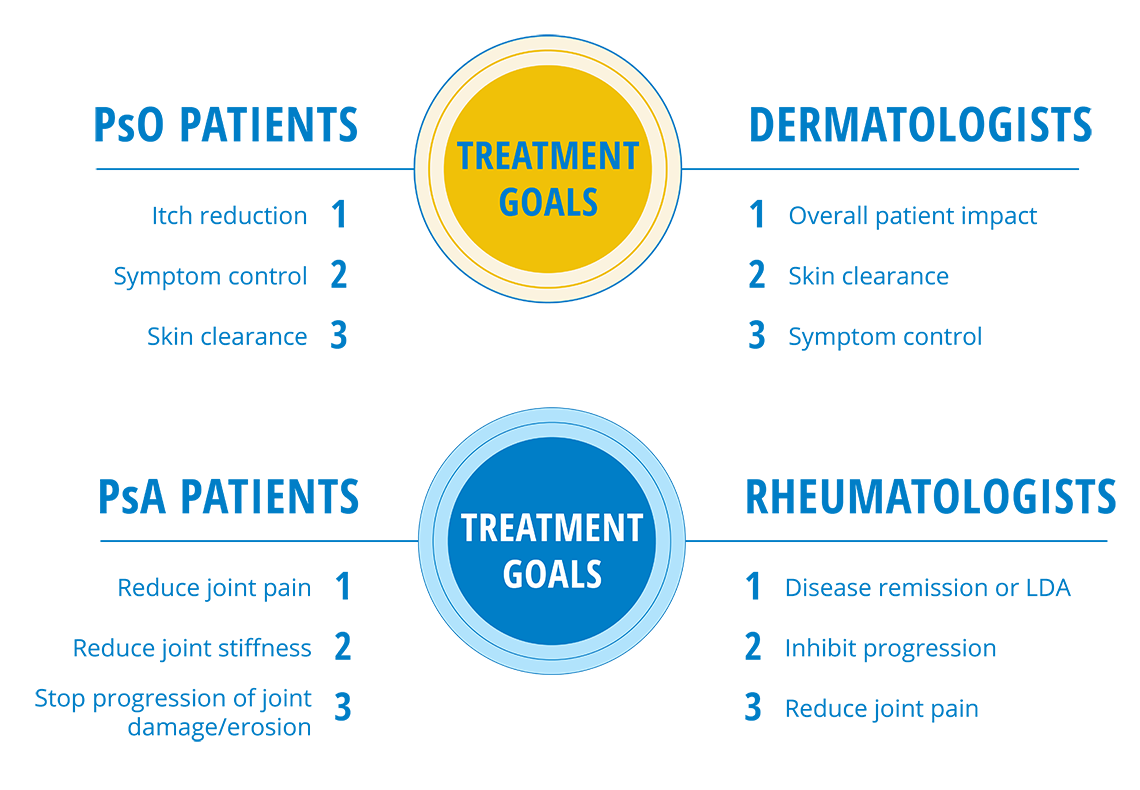
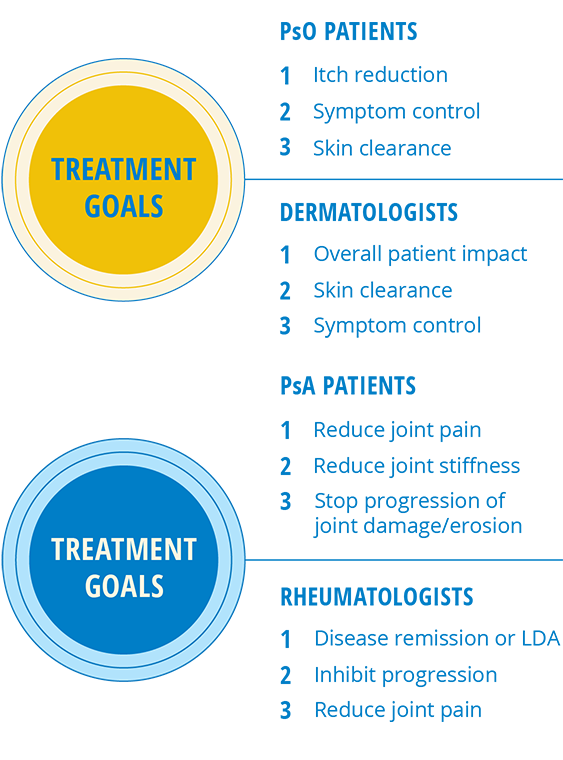
It can be hard to pin down what’s causing this disconnect between doctors and patients because everyone’s experience is different. But if patients are equipped to have more open conversations with their doctors and feel empowered to speak up on the treatment goals they want, how they view their own disease severity, their concerns around undertreatment, and more, they’ll be more likely to feel aligned with their doctors.

Missed Patient
Connections
So, what happens when a patient experiences a disconnect with their health care provider?
A missed connection, a feeling of being out of sync.
See how the real-life experiences of other people living with plaque psoriasis and psoriatic arthritis can help inform your conversation with your doctor.
Helpful
Patient Tools
Thankfully you can work with your doctor to help find what's best for you and your plaque psoriasis and/or psoriatic arthritis. Aligning your goals with the doctor's tools can help you have more meaningful connections.
The first step to feeling empowered at the doctor’s office is having the resources you need to have the right conversations. Our Helpful Patient Tools can help guide meaningful conversations with your doctor. From what questions to ask yourself and your doctor to how to assess where you are in your treatment journey, these tools may help you feel more prepared for your next visit.
Remember:
you can help bridge the gap between you and your doctor by having open and honest conversations.